Intermountain Health just presented research showing that personalized vitamin D3 dosing cut the risk of a second heart attack by nearly 50%.
Half.
Doctors adjusted doses based on blood levels — not a one-size-fits-all number — and patients got real results.
But here’s the problem:
Most EMRs treat vitamin D like a checkbox, not a dynamic treatment protocol.
Personalized medicine demands:
→ continuous monitoring
→ trend recognition
→ dose adjustment
→ and alerts when patients drift below target
Most documentation systems can’t do that at scale.
So the research sits on a slide deck instead of saving lives.
Until healthcare builds infrastructure that adapts as fast as the science, breakthroughs like this will stay stuck in the lab.
What’s the point of better evidence if we can’t operationalize it?
Intermountain Health just presented research at the American Heart Association’s Scientific Sessions showing that personalized vitamin D3 supplementation can cut the risk of a second heart attack in half.
Half.
The TARGET-D trial found that when doctors monitored blood vitamin D3 levels and adjusted doses to maintain levels above 40 ng/mL, heart attack survivors had roughly 50% lower risk of experiencing another cardiac event.
But here’s what really matters: 85% of participants started the study with vitamin D3 levels below that target threshold. And more than half needed initial doses around 5,000 IU to reach optimal levels.
The standard recommendation? 600 to 800 IU.
We’re talking about a six-fold difference. That’s not a minor calibration error. That’s a fundamental miscalculation about what patients actually need.
And it raises an uncomfortable question: what else are we getting systematically wrong because we’re built for standardization instead of personalization?
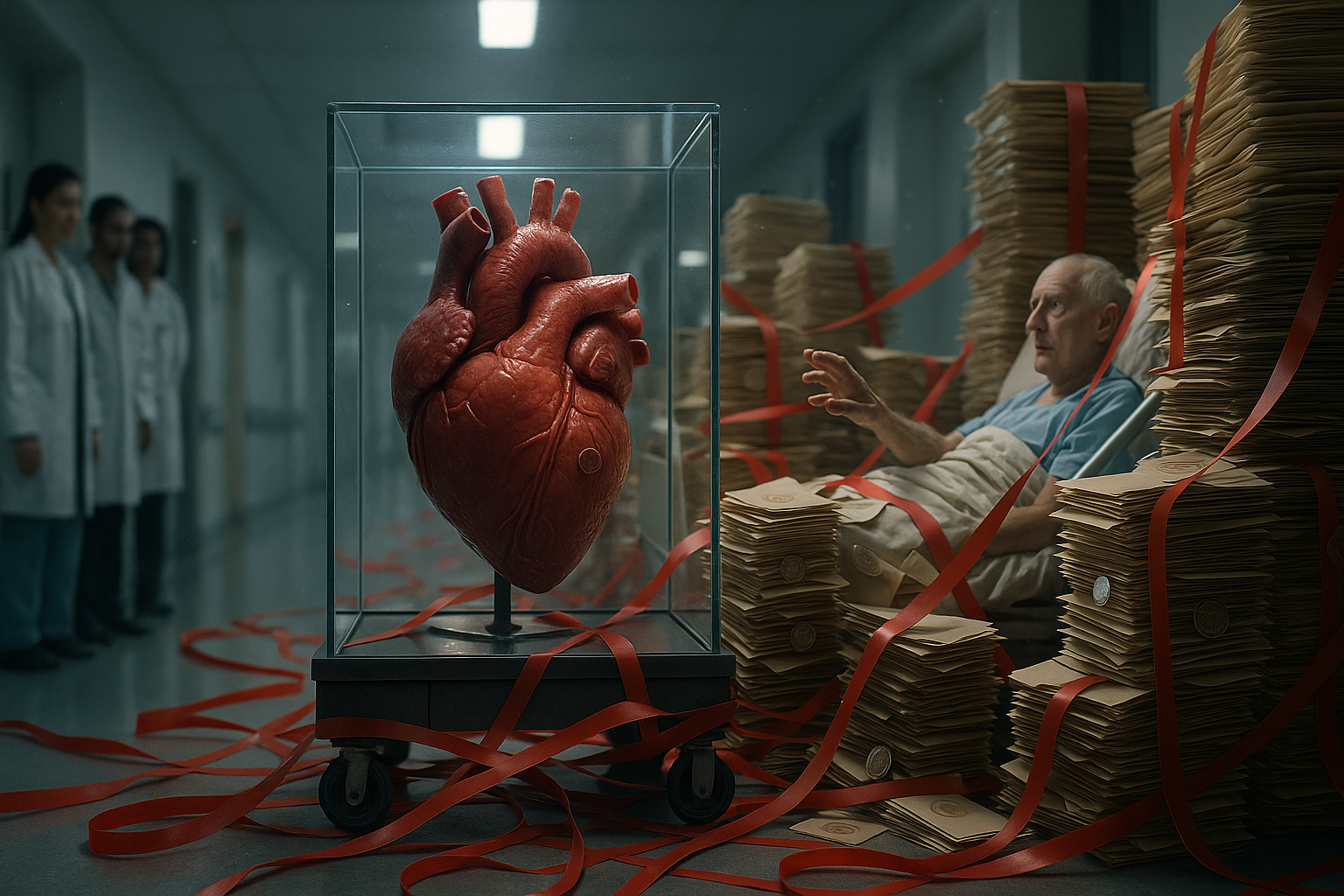
The Documentation System That Can’t Keep Up
Most EMR systems treat vitamin D as a checkbox item. You order it. You get a result. Maybe it flags if the level is critically low.
That works fine for standardized medicine.
But this research suggests we need something completely different. We need systems that track each patient’s baseline, calculate their individual target, monitor their response to different doses over time, flag when they’re drifting below 40 ng/mL, and prompt dosage adjustments.
That’s not a static data point anymore. That’s a dynamic treatment protocol requiring ongoing surveillance.
Here’s the problem: most documentation systems aren’t designed to handle that kind of longitudinal, personalized tracking at scale.
A cardiologist managing 200 heart attack survivors with individualized vitamin D3 protocols would essentially need a separate tracking system outside the EMR. Or they’d be drowning in manual chart reviews and spreadsheets.
The current setup assumes you prescribe something once and maybe check it annually. This research suggests we need continuous optimization. Our documentation infrastructure wasn’t built for that level of detail across large patient populations.
When Good Research Meets Bad Infrastructure
I’ve seen this pattern before with other personalized protocols. A cardiology practice tried implementing aggressive lipid management with specific LDL targets for each patient based on individual risk profiles.
Within three months, they abandoned it.
The clinical science was solid. The problem was operational chaos.
Nurses spent hours each week manually pulling labs, cross-referencing charts, creating reminder lists for follow-ups. The EMR sent generic reminders but couldn’t differentiate between a patient needing urgent adjustment versus one who was stable.
Providers missed patients who fell through the cracks because there was no systematic way to surface who needed attention.
They reverted to the standard protocol. Not because it was better medicine. Because it was the only thing their documentation system could support without consuming massive staff time.
Good research runs into bad infrastructure, and infrastructure wins.
The Two-Tier Problem Nobody Talks About
This vitamin D3 research is implementable. But only for practices that have already made significant infrastructure investments.
Large health systems with sophisticated documentation platforms and data analytics teams can absolutely do this. They can build custom tracking protocols, automated alerts, population health dashboards that surface which patients need intervention.
But your average cardiology practice? A small community hospital? They’re stuck.
And here’s what bothers me: this isn’t exotic medicine. It’s vitamin D3 supplementation and blood level monitoring. If we can’t operationalize something this straightforward without advanced infrastructure, what does that say about our readiness for truly personalized medicine?
The research is moving faster than our ability to document and manage it.
That creates a dangerous situation. Some patients get systematic, proactive management and benefit from that 50% risk reduction. Others don’t. Not because their doctors lack knowledge, but because their doctors lack operational capacity.
This is a clinical equity issue.
What Practices Actually Track Versus What They Think They Track
Most practices believe they’re tracking outcomes. What they’re actually doing is accumulating anecdotes.
Take compliance. A doctor orders vitamin D3 5,000 IU daily. It goes in the medication list. The EMR shows it as “active medication.” The practice assumes the patient is taking it.
But unless you’re systematically documenting follow-up conversations, checking pharmacy refill data, or tracking serial vitamin D levels over time, you have no idea about actual compliance.
You just know you told them to take it.
With personalized vitamin D3 monitoring, this becomes critical. The whole point is titrating to a target level. If a patient’s level isn’t rising appropriately, is it because they need a higher dose or because they’re not actually taking what you prescribed?
Without capturing true compliance data, you can’t distinguish between treatment failure and adherence failure.
But most documentation systems just have a checkbox: “Patient counseled on vitamin D supplementation.” That’s not data. That’s a liability shield.
The same thing happens with side effects. Practices think they’re tracking adverse events, but they’re only capturing what patients volunteer or what’s dramatic enough to trigger a call.
The subtle signals that someone’s not tolerating higher doses? That’s not systematically documented unless you have structured follow-up protocols.
So when a practice says “we tried personalized vitamin D3 management and it didn’t work,” what they often mean is “we prescribed personalized doses and didn’t see dramatic results.” But they don’t actually have the data to know why.
That’s the difference between anecdotes and evidence.
What Intelligent Documentation Actually Looks Like
Current systems run on scheduled reminders and population-wide alerts. “Patient is due for annual vitamin D check.” That’s calendar-based, not outcome-based.
What we actually need is intelligent exception surfacing. The ability to automatically identify which patients are deviating from their expected trajectory and need intervention, without requiring someone to manually review every chart.
Imagine a system that understands each patient’s individual target, monitors their trend, and surfaces exceptions: “Patient X’s vitamin D dropped from 45 to 38 ng/mL despite being on 5,000 IU. Possible compliance issue or absorption problem.”
Or: “Patient Y has been stable at 42 ng/mL for six months on 2,000 IU. Consider dose reduction trial.”
That’s not a reminder. That’s clinical intelligence.
It requires the system to know what normal progression looks like for each patient, detect deviations, and prioritize them by clinical significance. Right now, if you want that level of insight, someone has to manually review trends for every patient.
That doesn’t scale.
Personalized medicine generates exponentially more data points per patient. You can’t manage that with human chart review. You’ll miss things or burn out your staff trying.
You need the system to do pattern recognition and only surface what actually requires human decision-making. Everything else should run quietly in the background.
Without that capability, you’re just creating more work that practices can’t absorb. That’s why most personalized medicine initiatives fail at implementation. They add complexity without adding intelligence to manage that complexity.
The Accountability Question
But intelligent systems that do pattern recognition raise a critical question: how do you prevent that from becoming a black box where providers don’t understand why a patient is being flagged?
You can’t have a system making clinical prioritization decisions without transparent logic that providers can interrogate and override.
When the system flags a patient, it shouldn’t just say “Patient needs attention.” It should show the specific data points and thresholds that triggered the flag.
“Patient’s vitamin D level decreased 7 ng/mL over 8 weeks while on stable dosing. This exceeds the expected variation range of ±3 ng/mL and suggests possible non-adherence or malabsorption.”
The provider can see exactly why the system surfaced this patient and can agree or disagree with that logic.
More importantly, the system needs to learn from provider responses. If a doctor consistently dismisses certain types of alerts as not clinically significant, the system should adapt its sensitivity for that provider’s patient population.
That’s not the system overriding clinical judgment. It’s the system conforming to it.
Clinical accountability requires clinical autonomy. The system should surface what it thinks matters and explain why. But the provider makes the final call, and the documentation reflects that human decision, not just algorithmic output.
If you can’t explain why the system flagged something in terms a provider understands and agrees with, you haven’t built clinical intelligence. You’ve just built sophisticated nagging.
The Timeline Nobody Wants to Talk About
Let’s say this vitamin D3 research gets peer-reviewed, published, and eventually adopted into guidelines. What’s the gap between “this becomes standard of care” and “most practices can actually execute it”?
Three to five years minimum. And that’s optimistic.
You’ve got maybe a year for peer review and publication. Another year or two for it to make its way into clinical guidelines. Then the real delay: the operational implementation lag.
Even after something becomes “standard of care,” the average practice needs time to update EMR templates, train staff, build tracking protocols, and figure out workflow integration.
For something requiring ongoing monitoring and dose titration like this, you’re looking at significant infrastructure investment that most practices can’t just flip a switch on.
And what happens to patients in that gap? They get inconsistent care.
Early adopters start implementing it right away, even before it’s in guidelines. Their patients benefit. Everyone else waits. Their patients don’t.
You end up with tiered rollout where access to emerging evidence-based care depends entirely on where you happen to receive treatment.
The really frustrating part? This gap is largely artificial. It’s not about the science taking time to prove itself. It’s about operational systems taking time to catch up.
If practices had flexible, intelligent documentation infrastructure already in place, they could implement new protocols within weeks of evidence emerging, not years.
But most are stuck with rigid systems that require vendor updates, IT tickets, and committee approvals just to add a new tracking field. They’re perpetually behind the curve.
Patients in that gap are paying the price for our infrastructure deficit. They’re not getting inferior care because their doctors don’t know the research. They’re getting inferior care because their doctors can’t operationalize it.
The Trust Crisis Accelerating
We’re in a new reality where research gets presented at conferences, hits social media within hours, and patients are reading about it before their doctors have even seen the abstract.
The traditional gatekeeping model is broken. Evidence used to filter through peer review, guidelines committees, then slowly disseminate to practicing physicians. Patients aren’t waiting for that process anymore because they can’t afford to.
And I don’t blame them.
If you’ve just survived a heart attack and you see research suggesting a simple, low-cost intervention might cut your risk of another one in half, why would you wait two years for guidelines to update?
The information asymmetry has flipped. It used to be that doctors had access to research patients didn’t. Now patients often know about emerging evidence before their doctors do, but they lack the clinical context to interpret it properly.
That creates an impossible situation for providers. They’re getting asked about studies they haven’t had time to evaluate, being pressured to implement protocols their systems can’t support, and caught between evidence-based caution and patient expectations for immediate action.
Some doctors respond by dismissing patient concerns. “That’s not proven yet, let’s wait.” That erodes trust.
Others cave to pressure and implement things haphazardly. That creates safety risks.
The crisis isn’t just that systems move slowly. It’s that the gap between information availability and implementation capability is now visible to everyone.
Patients can see that the research exists, that it’s promising, and that they’re not getting it. That transparency is good in some ways, but it’s exposing just how dysfunctional our infrastructure really is.
We can’t hide behind “patients don’t know what’s out there” anymore. They know. And they’re rightfully asking why we can’t deliver it.
That’s the trust crisis. Not that we don’t have the knowledge, but that we can’t operationalize it fast enough to meet the moment.
The Misconception Blocking Progress
Healthcare leaders keep thinking personalized medicine is primarily a clinical challenge. It’s actually an operational one.
They ask “do we have enough evidence?” when the real question is “can we execute this systematically?”
I see executives investing in precision diagnostics, genomic testing, advanced therapeutics. All the clinical innovations. While completely underestimating the infrastructure required to actually use that information at scale.
They think if they train their doctors on the latest research and maybe add a few EMR fields, they’re ready for personalized medicine.
They’re not even close.
The vitamin D3 study proves this. There’s nothing clinically complicated about checking a blood level and adjusting a supplement dose. A first-year resident could manage it for one patient.
But managing it for thousands of patients, continuously, with the tracking and follow-up and dose optimization required? That’s an operational challenge without the right infrastructure.
And most leaders don’t see that coming until they’re already committed and drowning in it.
They think the barrier is physician adoption or patient compliance. The real barrier is that their documentation systems can’t support the workflow.
So they launch personalized medicine initiatives that fail. Not because the science was wrong or the doctors weren’t bought in. But because nobody thought about how a nurse would actually execute this on Tuesday afternoon with 47 other tasks on their list.
Until healthcare leaders start viewing documentation infrastructure as a strategic clinical asset, not just an IT expense or compliance requirement, we’re going to keep having this cycle.
Promising research that can’t be implemented. Frustrated providers. Patients who don’t get the benefit of what we already know works.
The misconception is thinking personalized medicine is about better science.
It’s actually about better systems.
What This Means for Healthcare Moving Forward
The Intermountain Health vitamin D3 research is still preliminary. It hasn’t been peer-reviewed. It showed no effect on stroke, heart failure, or overall mortality.
Those limitations matter.
But the research reveals something more important than whether vitamin D3 specifically becomes standard of care. It reveals that healthcare is generating evidence faster than it can operationalize it.
Previous vitamin D studies failed because they used fixed doses that were likely subtherapeutic. They didn’t evaluate therapeutic levels or adjust based on individual response.
The TARGET-D trial showed what happens when you do. You get meaningful clinical benefit.
But you also get a documentation and monitoring challenge that most practices can’t handle.
That’s the pattern we’ll see repeated with every advancement in personalized medicine. Better diagnostics. More precise therapeutics. Individualized risk stratification.
All of it generates more data points per patient. All of it requires more sophisticated tracking. All of it demands infrastructure that can surface the right information at the right time without overwhelming clinical staff.
Building Infrastructure That Keeps Pace With Science
This is exactly why we built MediLogix the way we did.
Not as another documentation tool that digitizes the same broken workflows. But as infrastructure that can actually support personalized medicine at scale.
When research like the TARGET-D trial emerges, practices using MediLogix don’t need to wait years for vendor updates or build tracking systems from scratch. They can implement new protocols within weeks because the intelligence infrastructure is already in place.
Our AI-powered platform combined with expert medical transcriptionist review doesn’t just capture what happened during an encounter. It monitors longitudinal trends, surfaces patients deviating from expected trajectories, and prioritizes interventions by clinical significance.
That’s not documentation. That’s the clinical intelligence layer healthcare has been missing.
For something like vitamin D3 monitoring, the system would track each patient’s baseline, flag those below target thresholds, monitor response to dosing adjustments, detect compliance issues through pattern recognition, and surface exceptions that need clinical attention—all without adding manual chart review burden to your staff.
The cardiologist managing 200 heart attack survivors doesn’t need spreadsheets or separate tracking systems. They get intelligent exception surfacing that tells them exactly which patients need intervention and why.
This is what operational capability looks like when it’s built for personalized medicine instead of retrofitted for it.
The Practices Already Prepared for What’s Coming
The healthcare organizations recognized as leaders in outcomes aren’t getting there through clinical expertise alone. They’re getting there because they invested in infrastructure that lets them operationalize evidence as it emerges.
They can pilot promising protocols systematically. They can generate their own real-world evidence. They can adapt quickly when research shifts.
That agility compounds. Every advancement in personalized medicine widens the gap between practices with intelligent infrastructure and those without it.
The vitamin D3 research is just one example. Tomorrow it’ll be a different biomarker, a different risk stratification tool, a different personalized intervention. The specific clinical question changes, but the operational challenge remains the same.
Can you track it? Can you monitor it? Can you respond to it systematically across your entire patient population without overwhelming your staff?
Most practices can’t answer yes to those questions yet. But they need to.
Closing the Gap Between Knowledge and Execution
The question isn’t whether this vitamin D3 research specifically pans out. The question is whether your practice infrastructure can evolve fast enough to support the medicine you’re already capable of delivering.
Because patients are reading about these breakthroughs before their doctors have time to evaluate them. They’re asking questions. They’re expecting responsiveness. And they’re losing trust when the system can’t keep pace.
That trust crisis isn’t about clinical competence. It’s about operational capability.
At MediLogix, we’ve watched healthcare generate breakthrough after breakthrough that never reaches patients because the infrastructure isn’t there to support implementation. We built our platform specifically to solve that problem.
Custom workflows tailored to each specialty. Seamless EMR integration that works with 99.9% of cloud-based systems. Automation across the entire patient encounter—pre-visit, during documentation, post-visit coding and compliance. Workflow analytics that surface exactly where intervention is needed.
This isn’t about replacing clinical judgment. It’s about building the operational scaffolding that lets clinical judgment operate at the speed and scale that modern medicine demands.
The practices investing in this infrastructure now won’t just implement the vitamin D3 protocol if it becomes standard of care. They’ll implement whatever comes next. And whatever comes after that.
They’ll deliver better outcomes. They’ll reduce clinician burnout. They’ll build stronger patient relationships based on trust that the system can actually respond to new knowledge.
The practices that don’t will fall further behind. Not because they lack clinical expertise. Because they lack operational capability.
That gap will only widen as personalized medicine accelerates.
The infrastructure deficit isn’t permanent. But closing it requires viewing documentation systems as strategic clinical assets, not administrative necessities.
It requires building for the medicine we’re moving toward, not the medicine we’re moving away from.
And it requires recognizing that the barrier between promising research and patient benefit isn’t scientific anymore.
It’s operational.
We’re solving that.